Feature: The vital role of antibodies in biomedical research
- Sep 7, 2020
- 5 min read
Updated: Sep 23, 2020
Antibodies, the small proteins which form a critical part of our immune response to disease, are the unsung heroes of much biomedical research.
And for decades the production of antibodies to counter and help us understand viruses - such as Covid-19 and many common infectious diseases - has relied on the use of animals. However, a debate has begun on how soon the biomedical sector will be able to move from the use of animals to greater reliance on non-animal methods.

How antibodies work
Antibody proteins are produced naturally by humans and animals after exposure to a foreign object, such as a virus, that has invaded the body. These antibodies are produced by immune cells, which recognise one small portion of the foreign object, known as an antigen. Whenever these immune cells then come into contact with the antigen, they can reproduce the specific antibodies needed to fight the challenge to the organism’s health.
In research, scientists can exploit this process and use antibodies to help researchers find the presence, or even levels, of specific proteins to help diagnose conditions. Antibodies, in particular monoclonal antibodies (see box below), which bind specifically to only one part of an antigen, known as an epitope, can also be used as a treatment, and have been effective in arthritis, cancer, and autoimmune diseases.
Producing antibodies
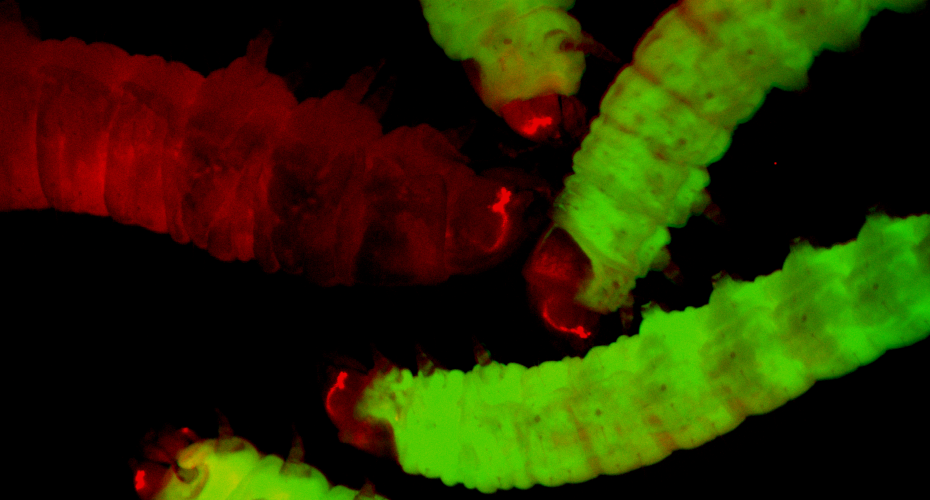
Antibodies can be generated in one of two ways. Currently, the majority of antibodies used in research are collected from animals and known as ‘animal-derived’. An animal, most commonly a mouse or a rabbit, although other animals are also used, is injected with a small amount of the desired foreign antigen, allowing the immune system to produce antibodies in response. These are then collected, either from the blood or from the spleen, for use in research.
90% of approved antibody treatments in the last five years are animal-derived.
Production of antibodies in response to a foreign body is one part of what’s known as the adaptive immune response, where cells can recognise and remember how to fight an infection they have seen before. How long this “memory” lasts depends on a number of factors, including how well the antibodies can identify the foreign object and how efficiently they stick to it. This response is specific to an individual's immune system, and can differ from person to person.
Advances with animal antibodies
Animal-derived antibodies are used in most areas of biomedical research, from understanding how a disease works in the body, to drug discovery and ultimately providing a treatment for patients. In particular, monoclonal antibodies developed using animal-derived methods have provided valuable treatment options for a number of diseases.
· Herceptin, a monoclonal antibody used in treatment of breast and colon cancers, was developed thanks to a study in mice, rats and hamsters and is now widely used as a targeted therapy for these cancers.
· RoActemra, used in severe rheumatoid arthritis, is a monoclonal antibody developed in mice and has been shown to slow progression of the disease.
· Ocrevus is a therapy developed using mouse antibodies, taken by patients with multiple sclerosis, and has been shown to reduce the number of relapses the patient will experience by up to 70%.
Antibodies and Covid-19
Most recently, the generation of antibodies using animal methods has been of critical importance in the global fight against Covid-19.
EARA members VIB, in Belgium, and the German Primate Research Centre, were able to generate specific antibodies against the virus, and demonstrated that they were able to neutralise the coronavirus in monkeys.
At Utrecht University, the Netherlands, a group used a mouse model exposed to the human virus to generate a specific antibody to allow diagnosis of Covid-19, and to block its infection of human cells.
The Karolinska Institute, Sweden, found that alpacas can generate a smaller-sized form of antibody against the virus, and that these are remarkably effective at preventing the virus from entering cells and thus causing infection.
In a similar manner, a collaboration between the University of Texas at Austin, USA and EARA members Ghent University, Belgium, found that llama antibodies could prevent the coronavirus entering cells, and have begun preclinical trials in order to develop this as a potential treatment for Covid-19.
Regeneron, a US pharmaceutical company, are using mice genetically engineered to have a human immune system to produce a cocktail of monoclonal antibodies preventing virus entry into cells, as a treatment for Covid-19 patients.

Developing non-animal antibodies
It is also now possible to generate antibodies using non-animal derived methods, thanks to developments of new technologies - one of which was jointly awarded the Nobel Prize for Chemistry in 2018. These methods involve inserting the genetic sequence of the desired antigen, originally sourced from a human or animal, into the DNA of a virus that solely infects bacteria, known as a bacteriophage, meaning it is able to produce the antigen.
This can be repeated for many different antigens and result in the creation of large libraries of bacteriophages displaying (known as ‘phage display’) different antigen sequences, which can be used to identify proteins.
In May 2020, a working group within the EU Reference Laboratory for alternatives animal testing (EURL ECVAM) published a report suggesting that the scientific community should move away from animal-derived antibody production methods entirely, in favour of these non-animal derived approaches.

“Animal-derived antibodies are plagued by efficacy issues, with repercussions for research reproducibility, diagnosis and health management,” said the agency in a Nature correspondence article published at the same time as the report.
The report stated that non-animal derived antibodies are not only available, but are preferable to animal-derived antibodies in terms of their shelf-life and the ease with which they can be replicated.
However, at an NC3Rs webinar on the topic, Dr Alison Gray, a member of the working group, acknowledged that it would take a lot of time and effort for institutions to establish their own full libraries of antigen sequences.
While the focus of the report is on the use of antibodies in identifying proteins and drug discovery, it also suggests that antibodies used for drug treatments should also be replaced by non-animal derived alternatives.
Although the report correctly points out, that in line with the Directive 2010/63/EU, it is necessary to move to a non-animal alternative when such methods exist, it remains to be seen whether such an immediate switch away from animal-based methods of antibody generation is actually possible.
"It is short sighted to presume that animal derived antibodies can be replaced by antibodies from other sources. Of course we will try to use antibodies from other sources but animal derived antibodies still remain an important requirement for a lot of our cancer research." (Netherlands Cancer Institute)
The EURL ECVAM statement that scientific funding bodies should refuse to fund projects that involve the use of animal-derived antibodies has raised serious concerns within the biomedical community. This is because it is still not clear whether non-animal derived antibodies are always comparable to animal-derived, and there are cases where there are simply no non-animal derived antibodies available as a suitable alternative.
In the long-term, establishing non-animal derived antibody libraries should result in the faster generation of antibodies and reduce the costs associated with animal housing, but, until they are fully in place it is likely that scientists will continue to rely on animal-derived antibodies to ensure the highest quality of biomedical research.